Moving Faster
Applying Modern Design to Prosthetics
The process for creating prosthetic devices is painfully slow and based on out-dated technology. Digital tools and 3D printing can change everything; they certainly did for Paralympic cyclist, Denise Schindler.
Images courtesy of Autodesk and Dezeen

By Paul Sohi, Product Designer, Autodesk
You may not know much about prosthetic devices. Chances are, unless you know someone who requires one, you haven’t given them much thought.
There are 2 million people in the US who require a prosthesis, with an estimated 185,000 people receiving an amputation each year. But the number of students going on to study biomechanics and becoming qualified prosthetists is declining. It’s a scary thought; we’re slowly marching toward a future where someone could be waiting years for a prosthetic device. This doesn’t even take into consideration children born without limbs, who often are not given a prosthesis in their infancy, as they grow so quickly they need new ones faster than a prosthetist can realistically produce them. This in turn means children who should be “prosthetic native” are not, and when they finally receive a prosthetic, more often than not, they prefer to simply not use the device as it isn’t natural to them — they find it cumbersome.

German Paralympic cyclist, Denise Schindler, discusses her first-of-its-kind prosthetic leg with President Obama and Chancellor Merkel.
Rooted in History
Modern prosthetic design has its roots in the 1500’s — and things haven’t changed much in 500 years. For upper and lower limb prosthetics, sockets — the part of the device that connects directly with the residual limb — their design has not evolved significantly from their early 16th-century predecessors. Initially these sockets were made of carved wood, now there is a standard process of plaster cast molding a limb and building a socket around that mold. The mechanisms that replace joints have remained largely crude as well, with spring lock mechanisms, hydraulics, and other relatively old mechanical techniques used to replace incredibly intricate and complex biomechanics like the human knee. Over time, plastics replaced wood, and now carbon fiber is slowly becoming the standard material for sockets.
Prosthetic technology is evolving too slowly and demand continues to rise. There are no standards of minimum acceptable criteria for prosthetic devices. Instead, each individual prosthetist determines performance and function on a case by case basis. With the high rate of demand and the lengthy process to fit, design, and produce a prosthetic device — each one a customized medical product — prosthetists can’t keep up.
Sadly the results of these problems are felt worldwide, with wait times for a prosthesis often lasting as long as six months, with no guarantee of a comfortable fit due to the analogue processes used to create devices. The body can also change enough in six months to render a new device largely unusable.
I’m not a prosthetist, I’m a product designer, but I’ve found myself specializing in prosthetic design. When I learned about the state of prosthetics and the lack of new technology, I won’t lie, I was angry — but that anger spurred me to action. No one in need of prosthetic care should have to wait for a device in the era of digital technology and 3D-printing. In 2015 I joined Autodesk, a software company that helps people make anything — and in my first week I was assigned a project in Germany with Denise Schindler, a Paralympic cyclist. Our aim: to explore whether it was possible to use digital technologies and processes to augment prosthetic creation, and wherever possible, replace analogue processes if it would mean a prosthetic device could be made faster and better.
Let’s get digital.
Before we talk about improving the process of creating a custom prosthesis, it’s important to understand the existing process. When a patient meets with a prosthetist, they have an initial consultation, then a plaster cast mold of their limb is created. This is a standard mold-making process reminiscent of plaster molds for ceramics. Because plaster shifts as it dries, a few molds are made, then filed and cleaned to ensure the most accurate cast of the residual limb.
My first attempt at modernizing the prosthetic production process involved using a $250 piece of equipment, a 3D scanner. With it we were able to produce an accurate three-dimensional model of Denise’s leg in less than fifteen minutes. In less than a day, we demonstrated we could radically improve the first step of the process — perhaps in the future prosthetists wouldn’t even need to bother with plaster!
There was cause to celebrate and it was time to assemble a team of great designers and engineers to take this initial success and turn it into a real solution for Denise. I was based in London, our prosthetists were in Nittenau, Germany, our Autodesk mechanical engineer, Taylor Stein was based in San Francisco; my intern, Myles Cooper was in Portland, OR; and our advisor, Mickey Wakefield, was in Munich. We had a team of experts working across the world, digitally synchronized, to redesign prosthetic care.

The Autodesk team created a detailed 3D scan of Denise’s leg to produce a better fitting socket in a fraction of the time.
Concept Car
As many product designers are apt to do, the next thing we did was produce a concept model; a visual prototype of a device that pushed the envelope with total disregard for budget or technology limitations. You often see this approach with concept cars. Car manufactures create a future concept and make it real enough to inspire the next generation of production vehicles.
The concept-car-prosthesis we showed Denise was lightweight — made from carbon fiber and polycarbonate — with smart textiles integrated into the socket. It had a removable, onboard computer that would give Denise real time feedback on her device’s performance. It even had “speed-holes,” which actually weren’t terribly aerodynamic we came to find. The concept model was beautiful. We set ourselves to making version one based on that vision, and we failed. We had 3D-scanned a limb, but that didn’t turn us into trained prosthetists overnight. Denise and her team schooled us on her particular amputation: the base of her limb is extremely sensitive, the flesh and muscle that grew there is very thin, and so even the mildest amount of pressure on it can be excruciatingly painful for her. In some areas we could innovate, and in this case we needed to figure out how to replicate what Denise’s prosthetists had mastered for her years ago: a socket that grips around the knee in a comfortable, but efficient way, to drive thrust down into the bicycle without causing Denise pain. Our version one socket didn’t cover nearly enough of Denise’s limb to make this possible.
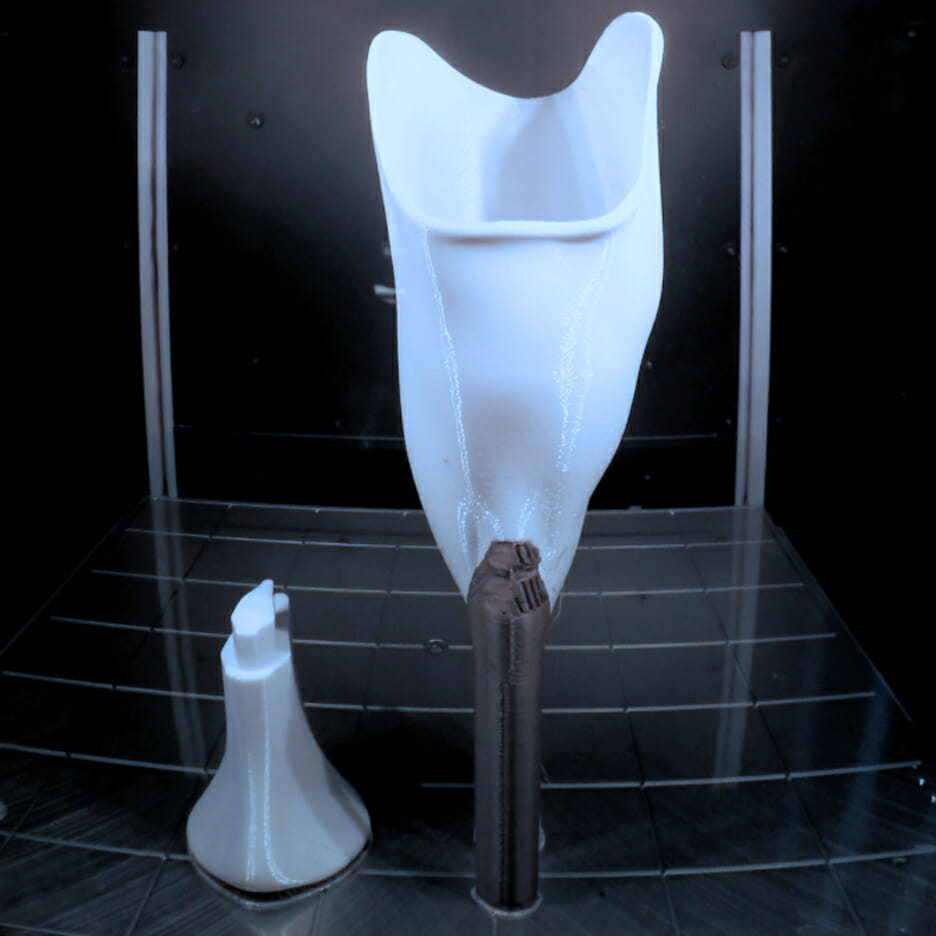
3D printing the prosthesis drastically reduced production time and created a device more reminiscent of our own natural biomechanics.
Stepping Up
In design, failure is merely iteration. We learned a lot in a short amount of time to design an effective, Olympic-level prosthetic device for Denise. But how to make it real? Prosthetic devices are a custom product every single time, they are not interchangeable between patients, and as we’ve established, they take a really long time to make.
Prosthetists are starting to use carbon fiber to make ultra-lightweight, durable sockets, but carbon fiber parts take time, and they are extremely rigid — the human body isn’t. We’re 60% water, so imagine what happens when you put an already sensitive amputated limb into an extremely rigid socket. Even with a silicone liner, sores, lesions, and bleeding can occur, especially for Denise who expels more energy on her prosthesis than most.
3D printing opened up many opportunities for us to address the time and rigidity issues. While carbon fiber is a uniform material — meaning it has the same thickness everywhere — 3D printed parts can be thicker in some places, thinner in others, more akin to our natural biomechanics. With this production technology we could analyze Denise’s driving forces, design a socket that perfectly aligned to those needs, and build a one-of-a-kind, comfortable prosthesis.
By December 2015, we created our first production model, a fully 3D-printed prosthetic device, with an intelligent socket. We used polycarbonate plastic, and utilized its natural material properties to produce a socket that was more flexible in areas where Denise needed comfort, and stiffer in areas where she could effectively drive force into the bicycle. The net result was a prosthesis that was more comfortable, without sacrificing performance, which for Denise meant being able to ride at maximum effort for longer.
Denise then did the one thing we asked her not to do: the very next day after trying this leg on for the first time, she took it to the velodrome and started training on it. We weren’t sure if it was going to stand up to the forces she would exert on it, we were in uncharted territory — no one had ever attempted to produce a prosthetic leg this way before! Thankfully it didn’t break, and Denise was setting new personal best times using the device.
As an added benefit for Denise, we designed the leg in two parts. She has the ability to remove the bottom piece and replace it with a longer element to adjust to different ride heights and bicycles. We also added an aluminum plate with threaded elements, which allows her to adjust not only the position, but also the attachment angle of her cleats to the pedals. We listened to the prosthetists too — Denise wears a special rubberized neoprene sock between her leg and the socket. A small vacuum cap on the back of the device creates an airtight seal — as her limb moves, any excess air is pushed out and can’t get back in, creating the best fit possible.

Never Stop Spinning
Between May and December 2015 we went from a team who knew next to nothing about biomechanics to a group that had produced a one-of-a-kind prosthetic device. This was all made possible by infusing digital technology and 3D printing into the process, and remaining informed by the deep knowledge of our prosthetist partners. We took a process with a normal lead time of 6-10 weeks and cut it into 10 days; producing a prosthetic that was only 200 grams heavier than its carbon fiber counterpart — and we still had nine months to iterate before the Paralympic Games in Rio de Janeiro.
Denise would always tell us to never stop spinning. We didn’t. Over the course of the next eight months leading into August, we would reach a total of 72 design iterations on the prosthesis, some minor, some major changes and refinements. At this point we had comfortably reproduced the process for creating a prosthetic device digitally, introducing virtual simulations to see how it would behave in the real world, testing the physics of the prosthetic itself, as well as rudimentary simulations that could give us an idea of how the prosthetic would perform for comfort.
Using 3D printing not only helped lay the foundation for a new process for masscustomization of prosthetics, it helped us reduce the overall weight of the device. Using a cutting-edge tool from Autodesk, Netfabb, we were able to intelligently design the inside of each 3D-printed part. Typically 3D-printed parts have a simple lattice fill technique, but we were able to add structure in some places, remove it in others — all informed by our digital and physical tests — to create a prosthetic leg for Denise that was as light as physically possible without compromising performance. This work even further reduced our production time.
The First Ever
In September Denise was on her way to Rio with her new prosthetic leg in tow, built from start to finish in less than 48 hours, costing less than $500, and ready for racing. She became the first Paralympian to compete with a fully 3D-printed prosthetic. Denise won silver and bronze medals in two events she had not medaled in before — the team and I were so proud.
I have been openly sharing our design and engineering techniques with every prosthetist interested, and am in the process of creating a series of videos, tutorials, and learning content on how to create prosthetics in the 21st century using digital tools and innovative fabrication. We need prosthetists to understand and utilize these techniques in order to solve the persistent issues in prosthetic care.
For myself and the team, the legacy of this project is what matters most. Denise continues to smash records and reigns as a world champion on a prosthetic device we made for her using a method that had never been tried before. We’ve trained numerous prosthetic studios and prosthetists in the methodology, and seen our work improved upon and modified in an explosion of creativity and problem solving. The future of prosthetics and medical hardware in general is only going to improve from here, and I am proud to have contributed to that future.
