Human Operating System
Design Thinking for Sustainable Healthcare

The U.S. healthcare system is dangerously complex — it is past time for design thinking to chart a new, human-centered course.
By Bill Hartman, Partner, Essential Design
The business of healthcare, which has the ultimate goal of sustaining wellness, is not on an economic trajectory anyone would call sustainable. Although expanding knowledge in life sciences and diagnostic technology has boosted therapeutic choice and overall sophistication, we continue to increase our spending on healthcare year over year. In fact, the U.S. spends more on healthcare than any other country — $9,237 per person per year according to a report in The Lancet (1).
Despite the highest costs in the world and flashy medical breakthroughs, the United States ranks 12th in life expectancy among the 12 wealthiest countries (2). Compounding this problem, the U.S. has fewer practicing physicians per capita and fewer patient visits per year than most other medically advanced countries. So where is the money going? We’re paying the most, and we have nothing to show for it except shorter, sicker lives.
We need a new system. Costs are increasing, but day-to-day delivery of healthcare hasn’t changed much. Design and innovation can play a critical role in creating and implementing an advanced, sustainable system that maintains a healthy equilibrium between costs, care, and services.
Follow the Money
An estimated 155 million people under the age of 65 are covered by employer-sponsored insurance. With healthcare costs generally covered by payers (firms) rather than patients (people), fee-for-service continues to be most prevalent business model, but it naturally creates disincentives and market failure. Healthcare providers will routinely over- service patients as reimbursements incentivize more procedures per patient than necessary. Layered on top of all this is the expensive and complicated administrative overhead within a messy ecosystem of providers, brokers, and insurance companies.
Additionally, shortages of primary care physicians, particularly in rural areas, have shifted people to expensive emergency care, and in some cases, precipitated chronic dependencies on pain medications — resulting in more unintended consequences at even higher costs – both financial and social.
And as we’ve disconnected the patient from paying directly for healthcare, some believe we’ve inadvertently eroded patient accountability and negatively shifted lifestyle choices: why be healthy when your employer-sponsored health insurance will cover your treatment, complete with a range of pharmaceutical options?
The United States spends more on healthcare than any other country: $9,237 per person per year.
New Models
A fee-for-patient model, also known as value-based care, aims to combine the accessibility of single-payer healthcare with free-market cost efficiency. In this case, providers lose the item-by-item reimbursements for services rendered, but they also remove the high-profit motive of insurers — often a barrier to providing most efficient, necessary care.
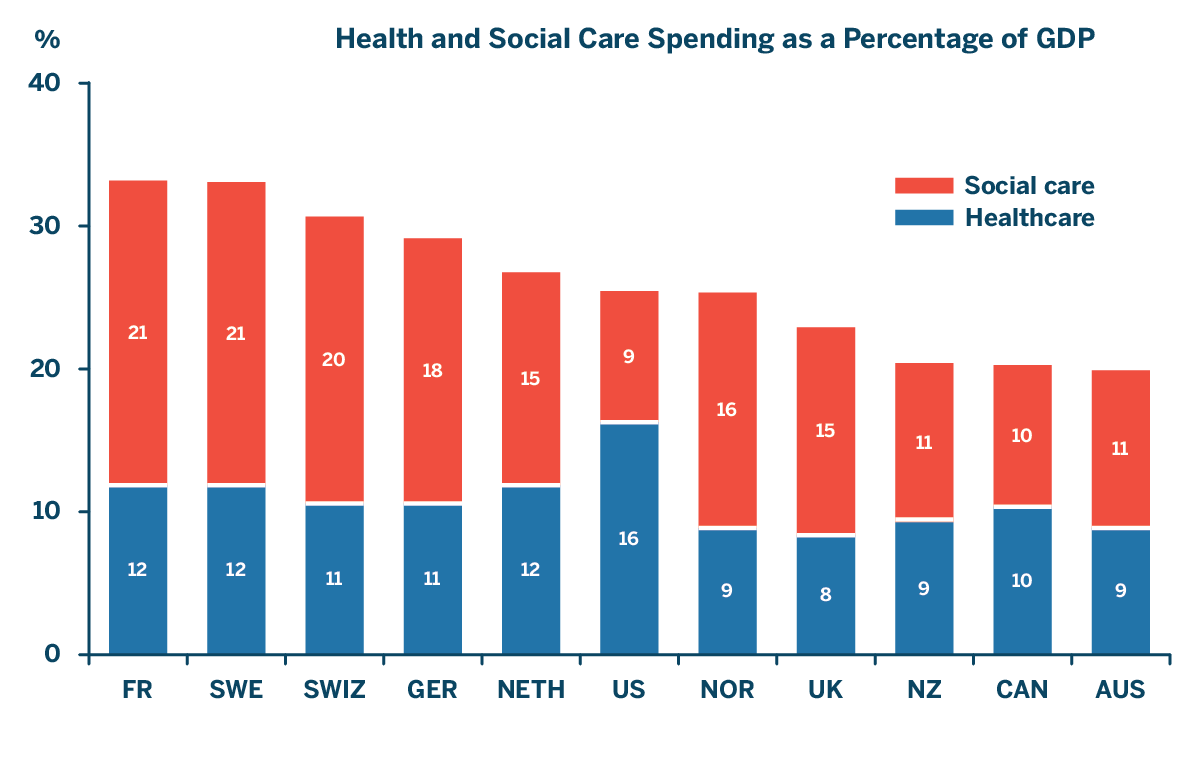
A study by the Commonwealth Fund offers a growing body of evidence showing that social services, lifestyle, and environment play important roles in shaping health trajectories. Other developed nations exhibit higher investments in social services than the U.S. and experience overall better health (3). Is there a connection? The study speculates that new care models rewarding healthcare providers based on patient outcomes creates a business case for providers to invest in certain social services and non-clinical preventive care versus costly medical procedures and medication once things go wrong.
MassHealth, the state of Massachusetts’ healthcare insurance program, observed a reduction of $2.50 in healthcare costs for every $1.00 invested in social services. More broadly, health reform in Massachusetts is credited with reducing emergency department visits and non-urgent visits by 1.9% and 3.8% respectively; significantly reducing deaths from causes amenable to healthcare; and reducing the amount of patients’ healthcare debt. A new healthcare model can have implications extending well beyond the health of those who gain insurance coverage. Dr. Jay Parkinson, Founder of Sherpaa, a new genre of healthcare delivery, put a fine point on this, observing that “most healthcare problems aren’t medical, they’re social.”
At Essential Design, we’re tracking psycho-social trends intersecting health and wellness. With mandates for more healthcare efficiencies, design plays a role in addressing a range of problems, often with competing variables. We can look to service design principles and the thoughtful incorporation of behavioral science to synthesize new solutions from disparate, inefficient parts.
Design for Improvement
What can be done to improve outcomes? What patient-centered opportunities exist to control costs? How can we collect and use data to make change proactively rather than reactively? We have some ideas to make understanding the process and evolution of healthcare a little easier.
Keep patients in closer orbit. I’ve heard it said that healthcare in the US isn’t really healthcare — it’s sickness-and-death-care. We must move away from the break-it-fix- it mentality and move toward prevention, wellness, and accountability across the system. Take nutrition — instead of costly medical procedures and pharmaceuticals, perhaps we should subsidize healthy, natural foods to combat and reverse alarming trends in diabetes and heart disease. This is an opportunity for designers and medical professionals to develop systems, services, and products that empower people to be healthier. We must think of healthcare as a human operating system in which each component plays a part over time rather than as a collection of disjointed transactions.
Mutually beneficial engagement. Shifting the provider-to-patient service dynamic toward one of shared value and effort benefits both parties. Accountable patients not only experience better outcomes but also incur less cost, helping the entire system to be more efficient. Patients who become students of their conditions generally fare better within the healthcare system because they ask questions and advocate for their own care. These self-directed patients are more mindful and actively develop better strategies for symptom management in collaboration with healthcare providers. They also, in many cases, become natural advocates for other patients with the same conditions. A great example is PatientsLikeMe, an online platform for patients to connect and learn from others like them and where researchers can learn more about what’s working and what’s not. We should design and launch more platforms, education programs, and services to help patients fully understand and own their wellness.
People-centered. Progressive Insurance’s Snapshot program rewards safe driving habits through discounted premiums. Health insurance companies have long charged higher premiums to smokers. It’s imperative that we develop incentive programs that encourage health and wellness. Some programs exist, like the rewards some insurers provide for joining a gym. Our health plan at Essential offers $300 simply for having primary care doctors submit a health status report to the insurance company — this is usually simply a matter of scheduling a routine, and free, physical exam. Through our design work in this space, we’ve discovered that the stickiness of these programs improves with emotional and social ties. This led us to explore the possibilities around a member toolkit — a manual highlighting available services and ways to boost overall engagement in a patient’s wellbeing. We also helped MeYou Health develop a series of personal wellness mobile apps leveraging social networks and delivering ongoing health knowledge and relevant action plans.
Third wave of digitization. Most people know more about the performance of their car or the details of the retirement plan than they do about their own bodies — because in the former two instances there is real-time data and visualized feedback loops. Another example: homeowners who can view their electricity consumption and compare it to their neighbors in real-time typically change their energy-use behaviors to align with best practices. For our new human healthcare operating system to be successful and efficient, we need more tools for capturing and displaying data that can lead to clear calls to action for each individual person. Biomarkers, measurable indicators of a biological state or condition, are currently used by healthcare professionals to monitor chronic illnesses, providing useful, quantitative data on which to base decision making. The economic pressures involved in value-based care will lead to biomarkers, sensors, and other real-time data capture methods to be part of our everyday lives. The Internet of Things will inevitably become part of our bodies and provide a constant awareness and connection between our lifestyle choices and our health.
Source: E.H. Bradley and L.A. Taylor, The American Health Care Paradox: Why Spending More Is Getting Us Less, Public Affairs, 2013.
Customized Future
Designers, who are collectively demonstrating high interest in problem-solving for social causes, can dramatically influence the path of healthcare toward the greater good. The work to customize outcomes has already been completed in other industries. Online markets have developed sophisticated algorithms to address specific market niches — if you bought this, you’ll also like this. Rapid customization allows users to deliberately create profiles and preferences based on their needs — needs which are then organized by algorithms, and then catered to through digital, and now physical, automation. Admittedly, marketing and healthcare have fairly different tasks, but perhaps we can create and service health markets of one, for each individual person. Using design skills, processes, and tools, we can set a new precedent and create a healthcare operating system for healthy and happy Americans. Let’s crack the code.
Bill Hartman is a Partner and leads the Innovation Strategy group at Essential Design, a firm providing Product, Service, and Digital expertise to help clients create breakthrough customer experiences. Also an Adjunct Lecturer at Bentley University, Bill’s interests include structured approaches to framing human-centered design goals, connected product portfolios, and optimizing platforms. In his free time, he applies behavioral economics to helping furniture and cats co-exist.
Sources
- Dieleman, Joseph. “Evolution and patterns of global health financing 1995–2014: development assistance for health, and government, prepaid private, and out-of- pocket health spending in 184 countries, The Lancet, 20 May 2017, http://www.thelancet.com/journals/lancet/ article/PIIS0140-6736(17)30874-7/fulltext.
- Brink, Susan. “What Country Spends The Most (And Least) On Health Care Per Person?” NPR, NPR, 20 Apr. 2017, www.npr.org/sections/ goatsandsoda/2017/04/20/524774195/what-country- spends-the-most-and-least-on-health-care-per-person.
- Anderson,Chloe and Squires, David. “U.S. Health Care from a Global Perspective.” Spending, Use of Services, Prices, and Health in 13 Countries, The Commonwealth Fund, 8 Oct. 2015, www.commonwealthfund.org/ publications/issue-briefs/2015/oct/us-health-care- from-a-global-perspective.