It’s Time for Open Source Healthcare
We must set healthcare free.
Designers can and should shape the future of healthcare, from how products and systems work to the underlying infrastructure and standards these products and services are built upon.
Images Courtesy of GoInvo

By Juhan Sonin, Jennifer Patel, and Jonathan Follett
Thoughtful design in healthcare, whether directly or indirectly impacting patients, can ultimately save lives.
Digital health promises that patients will have care plans and treatments best suited to their needs. We can deliver on that promise, but we’ll have to face some uncomfortable truths about our current system and fix them before we can get there.
Too often in the United States, health and the design of healthcare systems are treated like fashion, with an eye towards short-term profits and benefits rather than long-term sustainable infrastructure and patient-centered outcomes. Stewart Brand’s concept of pace layering aptly illustrates the problem under consideration: Fashion, the top layer, moves quickly and ephemerally, but culture, much slower to change, is bedrock principle. There’s a need for a better model, a better culture, that supports a longitudinal outlook and enables people to manage their health in conjunction with doctors, nurses, and other providers.
The Culture of Open
Anyone can change and share something that is open source because it’s publicly available under a generous license. While open source had its origins with computer code, it now influences how projects and businesses work. We benefit, often without realizing it, from this open sharing. Open source has grown into a culture of participation with many others that asks for transparency, community-based collaboration, and meritocracy. The best ideas float to the top, and you earn trust by what you do and how you amplify the group. Open design has succeeded in shaping technology, sustainability, and even humanitarian efforts.
Successful open standards, protocols, and services already exist, and they’re available on a global scale. We’ve developed them for critical elements of our economy, including finance, transportation, and digital communication. Web and mobile services were developed on, evolved on, and live on publicly-funded, standardized technology and infrastructures. Perhaps the prime example of successful open source in action, our Internet is infused with open source ideas and services, from how cell phones communicate to Linux to how e-mail is directed from one person to the next. All of these technologies working together are the operating system of the Internet.
So why are open standards not the norm in healthcare? Here in the United States in 2019, healthcare is sometimes amazing, often lifesaving, always expensive, and mostly closed. But it’s also territorial at its core, which means that each hospital, each doctor, each healthcare system invents its own way, to the detriment of our collective health.
It is common practice for health products to be locked down, closed off, patented, and sold for profits. Healthcare providers, including hospitals, clinics, and clinician organizations, own our data and keep business by not standardizing that information, making data ingestion from another organization painful. Even hospitals often have trouble reading data from installation to installation, which leaves third-party services, open or closed, out of the loop.
Surprisingly, many in healthcare actively rally against standardization, from individual doctors thinking their own way is best (as opposed to drawing on collective data across medical practices) to hospitals and other healthcare organizations preferring to devote their resources to developing their own research and treatment regimens. They are trusting their own ways more than already existing, proven solutions from other providers, solely because they were “not invented here.”
We spoke with Eric Topol, M.D., author of The Patient Will See You Now and leader of the Precision Medicine Initiative, on national standards for healthcare data:
“Data should not be put into a siloed environment in proprietary software systems,” says Topol. “Let’s go back to when the U.S. put $40 billion towards health information technology, when they never had the teeth to tell companies that we all need common data requirements and standards that are completely open and transparent, that lead to a more seamless data source. Why didn’t we do that? What is the problem in this country, where we don’t force all companies that are active in Health IT to have these standards? Only in recent times have we seen a bit of a push towards that, but it’s taking seemingly forever to get there.”
“We want each individual’s data from prenatal all the way throughout their life,” Topol continues. “All these things need to be accessible so that any healthcare clinician, with the patient, will have access to all this data instantaneously. Your life data and its easy availability for the care team are what we should aspire to and eventually achieve.”
The Future of Health is Open
We now need open standards for healthcare because our lives depend on it. Healthcare in the United States is among the most expensive in the world, from costs to the nation to the expense to the individual, and yet struggles to deliver quality care to patients. Open source can help healthcare be more standardized, more interoperable, more affordable, and more accessible for patients with limited access. Further, the open-source model is consistent with the philosophy of sharing best practices and innovations in care delivery to improve health, with benefits for individual patients as well as the entire population.
How might open source change our health system? First, open standards in healthcare empower and promote interoperability. Without open standards for health information, hundreds of different healthcare IT systems are currently unable to communicate with one another. This insular approach wastes up to $77.8 billion per year in the United States alone, in addition to causing medical errors and stifling research. Using open standards to improve health information networks and electronic medical record systems will allow patient data to become more portable between healthcare providers than it is today, ensuring more accurate and efficient care for patients.
Development of non-proprietary healthcare standards will create incentives for the providers of commercial healthcare IT products to adopt models of compatible data exchange and information systems; adopting open standards will open a path for them to stay competitive. At the same time, having open source software options will free healthcare providers from being locked in with one vendor and offer the added benefit of allowing them to customize the software to their specific clinical workflows and needs. With open source healthcare IT solutions, regions with limited resources that cannot afford expensive proprietary solutions will still have options for quality software to deliver quality care.
Design for Health: People First
There are many examples of open-source design projects in healthcare, from policy to strategy to user experience.
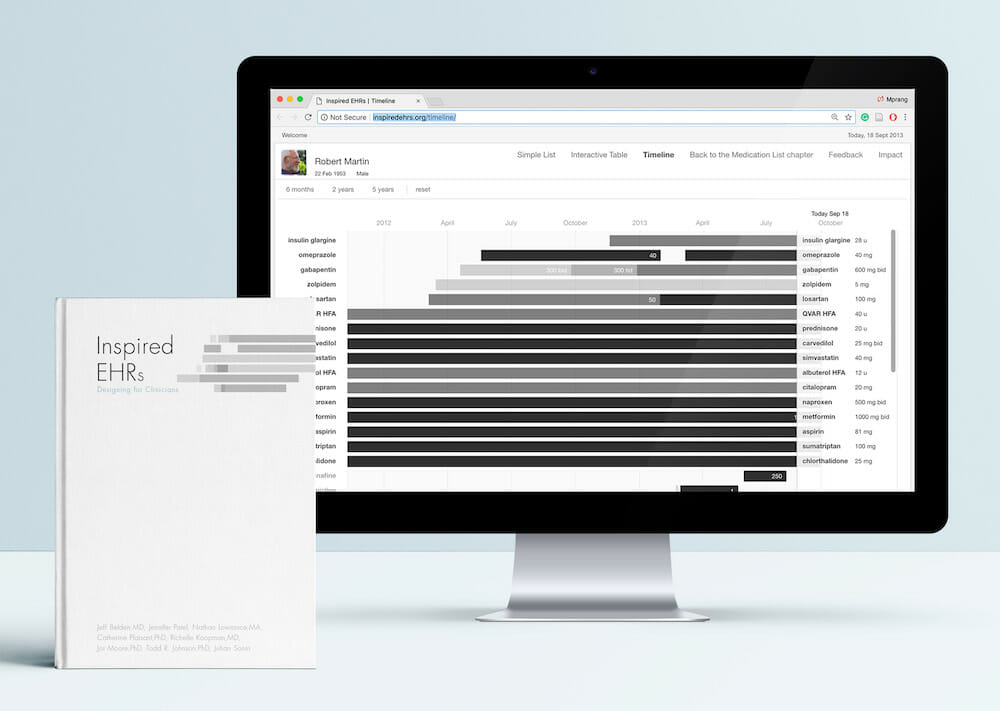
Inspired EHRs
Creating, updating, and reconciling medical records is one of the most visible areas where technology has shaped healthcare. While most electronic health record (EHR) systems remain proprietary, over 30 countries now use open-source EHRs in some capacity. Founded in a rich legacy of global initiative to meet shared, human needs, successful open-source healthcare IT initiatives are not only taking a hold in the United States, but also spreading to Mexico, Thailand, France, Uganda, Zambia, Kenya, Canada, Germany, the UK, Australia, Haiti, and many others.
However, current electronic health records are characterized by clumsy interfaces, poorly designed information, and cumbersome workflows, all of which distance clinicians from quality patient care. In most cases, these systems are set up for failure — clinicians for burnout, and patients for health risks.
With a team of physicians, nurses, health IT, and human computer interaction experts, GoInvo designed and co-authored an open source e-book to distribute ideas, designs, and techniques to health IT and EHR vendors to jumpstart EHR design on a national level. The result of the project was a lightweight, accessible, open-source design policy.
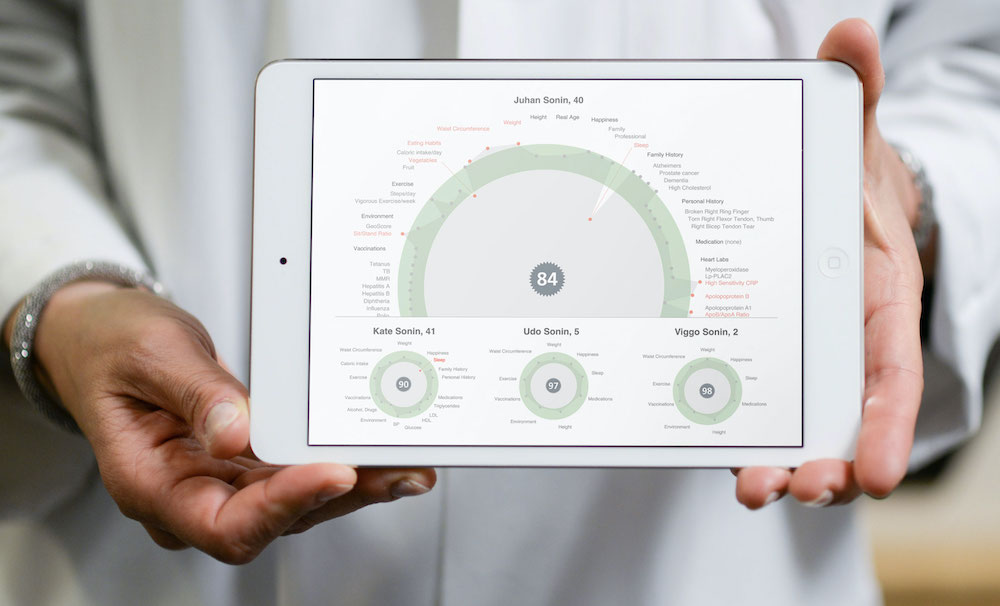
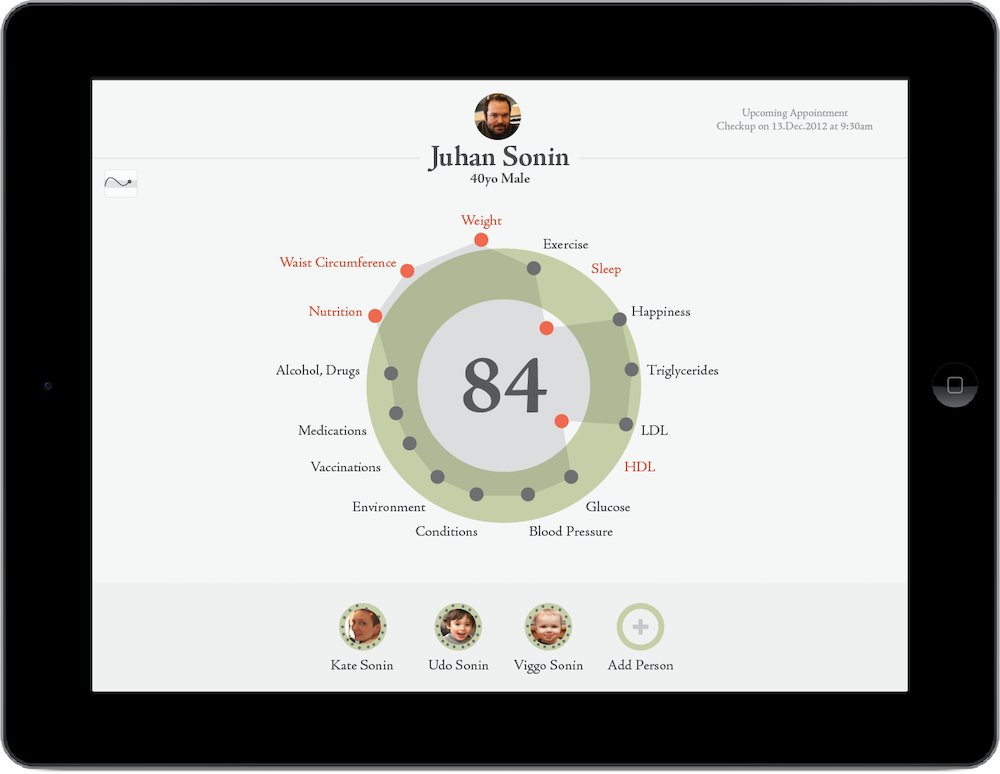
hGraph
Healthcare data is expected to grow between 1.2 to 2.4 exabytes per year. That’s about 1,000 times the amount of data the human brain is capable of storing. This data is big, disparate, and unstructured, making the identification of useful information almost impossible. In order for patients and healthcare providers to make actionable decisions, they need analytic tools that both collect data and make sense of it.
hGraph displays a considerable amount of health information in a deceptively simple fashion and in a small space. Through its shape and use of color, hGraph helps physicians to swiftly spot problem areas while retaining context of rest of the patient’s health.
It can display everything from behavioral patterns to test data, giving the viewer a complete picture of a patient’s health. The visualization aggregates health data both on a personal and community level. It provides clinicians with at-a-glance analytics of a patient’s overall health, allowing doctors to spot patterns and red flags. It works by comparing a person’s health data against targeted health ranges based on factors like age and gender. hGraph is an open-source tool that has been adopted by organizations including Walgreens, Crossover Health, NextGen, and Citizen Health.
Changing a Culture
When designing for health, designers must stick to medical regulatory compliance, but it’s also important to strive for more effective and ethical solutions. The ideas presented in this framework encourage the design of open systems and services for the responsible use and management of patient health data and information for the advancement of health quality, health research, and data ownership.
1. Simple National Standard
Designing from a single health data standard allows for a common data element definition for human health that works in systems across the nation, and ultimately for the world. This allows for systems to be open to talk to one another, empowers patients to take hold of their personal health data, and limits proprietary data vaults where decisions are made by a small circle of stakeholders.
2. Cost Transparency
Fight for prices of healthcare services, from medical treatments to insurance costs, to be publicly known and posted. Cost transparency promotes patient choice.
3. Responsible Use
Build ethical oaths and strong data use agreements for anyone handling patient data, such as researchers and third-party data analysis, to discourage and criminalize the unethical and wrongful use of personal healthcare data.
4. Data Usage Transparency
Design health receipts that a patient can take away and understand for every update or change to their healthcare record. After an encounter, a receipt detailing the conversation and collected information should be sent to the patient and corresponding care team. A health receipt will promote health literacy and engagement, allowing patients to understand and have a record of their health so that they can better apply it to how they live.
5. Transactional Care
Create open and transparent feedback for patients to see who, what, where, when, and how people and services use their healthcare data.
6. Patients Should Own Their Data
Include patient data ownership in every product and service, providing the patient with agency and choice when it comes to their health and personal information. Patients should co-own or fully own every health data point about themselves. Health data generated about the patient by a provider is co-owned by both parties. Health data generated by the patient is fully owned by the patient with a right to possess, share, sell, or destroy.
7. Data Should Be Shared
Allowing patients to share their personal health data at their discretion can improve the care they receive from health providers and enables more people to participate and contribute to health research. Patients should be free to use their personal health data in any legal way they choose and free to share some or all of their personal health data with whomever they choose.
8. Health Data is a Public Resource
Design and build systems and services that encourage citizens to participate in public programs like the census, so that individuals, companies, and governments can better predict on a national level health, regulation, and policy impacts on the needs of its citizens. Synthesized population data tools can improve public health, advance scientific research, and accelerate scientific and medical legislation.
9. Community Engagement
Design effective health education into products, services, and culture to develop a national health literacy for residents to absorb, starting at an early age. National health literacy drives the adoption of health data models and engages the imagination of the public to understand patient rights and health policy.